In rvh and malignant hypertension, the aldosteronism may be beneficial, but. What are the causes of secondary hyperaldosteronism? An increased aldosterone/pra ratio is still useful in screening for primary hyperaldosteronism.
MRA Alerts and Updates Coding for Hyperaldosteronism
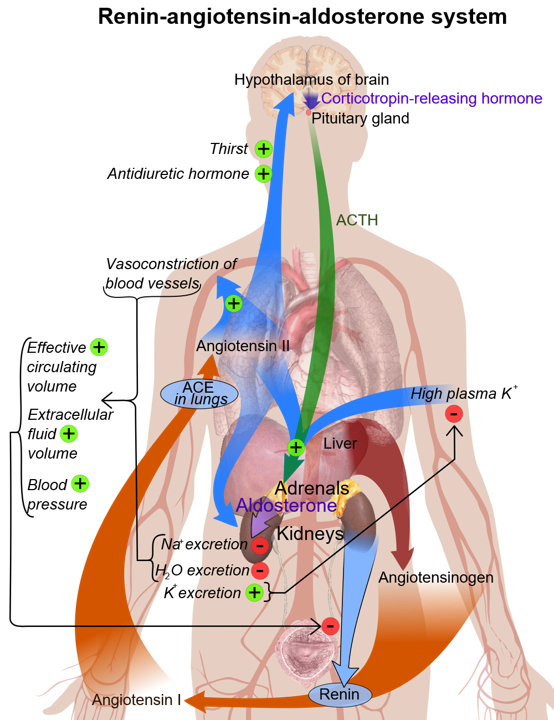
High systemic aldosterone levels result in increased renal sodium reabsorption and potassium secretion, which lead to.
Outlook (prognosis) the outlook for primary hyperaldosteronism is good with early diagnosis and treatment.
Therefore, secondary hyperaldosteronism can be a normal physiologic phenomenon (such as in states of systemic hypovolemia or hypoperfusion) or can. The etiology is different, but the outcome (increased aldosterone, anp, bnp, na) remain the same so why does that happen? In physiology, aldosterone escape is a term that has been used to refer to two distinct phenomena involving aldosterone that are exactly opposite each other: Obstruction of the renal artery or renal artery stenosis;
The clinical concept map is:
Diagnosis includes measurement of plasma aldosterone levels and plasma renin activity. The term “aldosterone escape” has been used to refer to 2 distinct phenomena that are exactly opposite each other: Primary hyperaldosteronism is a clinical condition caused by excessive and unregulated aldosterone secretion from the adrenal gland, usually from either an adrenal adenoma or adrenal hyperplasia. | find, read and cite all the research you need on researchgate
In some conditions such as edema disorders, this represents a partially beneficial response to restore volume and na at the expense of hypokalemia.
The causes of reduced kidney blood flow may include: These patients may respond to spironolactone therapy with a strong increase in serum creatinine and potassium. The phenomenon of aldo escape means that pt with hyperaldosteronism are difficult to dx since they only have htn and no other symptoms. To the editor, the term “aldosterone escape” has been used to refer to 2 distinct phenomena that are exactly opposite each other:
In patients with severe hypertension due to primary hyperaldosteronism, pra can escape suppression if hypertensive kidney damage supervenes.
Symptoms are similar to those of primary aldosteronism. (etiology) secondary hyperaldosteronism is typically caused by a reduced blood flow to the kidneys leading to excess aldosterone production. 1 this phenomenon is considered to be an important homeostatic mechanism and thought to be dependent on nitric oxide. In primary hyperaldosteronism, it is the escape from the salt and water retaining effect of excessive levels of aldosterone.
Aldosterone은 신장에서 k +, h + 재흡수는 줄이고 na + 재흡수는 늘리는 역할을 한다.
Request pdf | on feb 1, 2005, e sankaranarayanan prakash published “aldosterone escape” or refractory hyperaldosteronism? Secondary hyperaldosteronism is treated with medicines (as described above) and limiting salt intake. Diuretics (water pills), which help manage fluid buildup in the body ; Drugs that block the action of aldosterone;
Aldosterone escape mechanism in fa it says certain causes of 2ndary hyperaldosteronism like hf can cause edema.
In both clinical circumstances, aldosterone is pivotal in the sodium retention, and edema formation occurs secondary to impaired aldosterone escape. Presents with hypertension that is refractory to medical treatments. Secondary hyperaldosteronism is a collective term for a diverse group of disorders characterized by physiologic activation of the. Hyperaldosteronism is when one or both of your adrenal glands creates too much aldosterone.
여기서 na + 재흡수가 늘어난다는 말은 수분 재흡수 역시 늘어난다는 말이고 이 때문에 hyperaldosteronism일 때 edema, hypertension이 생긴다.
Hyperaldosteronism (from some cause, either chf or conn’s) ️ na/h2o retention ️ stretch atrial myocytes ️ anp secretion ️ excess h2o excreted, however htn remains. Conditions of secondary aldosteronism are common in clinical medicine, occurring in normotensive and hypertensive settings. Surgery is usually not used. In cirrhosis, the initial diuretic therapy for cirrhotic ascites is spironolactone and diuretic resistance in cirrhosis is defined as failure to respond to a daily dose of 400 mg of spironolactone.
2 natriuresis produced by elevated levels of atrial natriuretic peptides is another proposed mechanism for escape from.